15. Custodial Deaths
16. Dead brought to the Accident and Emergency Dept / MI Room (Found dead) and deaths occurring within 24 hours of hospitalisation without establishment of a diagnosis
17. Death on Operation table or Unexplained ICU death
18. Patient sustained injury while in the Hospital
19. Sudden death of patients after parenteral administration of a drug or medication
20. Unexplained death after surgery or during any interventional procedure
21. Admitted patient is not found in hospital premises, and when discharged in absentia- local police should be informed
22. Patient treated and then referred from a private hospital or other Government hospital with
complications of surgery or delivery or bleeding, where the cause of death is unexplained
23. Relatives of the patient assault the treating doctor or other staff of the hospital or creating another law and order problem in the hospital
GUIDELINES FOR DEALING WITH MLC:-
i. In emergencies, resuscitation and stabilisation of the patient will be carried out first and medico legal formalities may be completed subsequently. The consent for treatment is implied in all emergencies.
ii. The next important duty is to identify, after carefully analysing the injuries on the person of the patient, the history given, and the other circumstances of the case; whether the said case falls under the category of an MLC or not.
iii. If the case falls under the category of MLC, then he must register the case as an MLC and/or intimate the same to the nearest police station, either by telephone or in writing and also to his superior through official channel if he is in government service.
The Duty Constable at the Police Station should be informed about the name, age, sex of the patient and the place of occurrence of the incident. Every service hospital falls under jurisdiction of police station and the contact number should be available to DMO and in MI Room.
Local Police should also be informed regarding the discharge/death of the said patient in the Casualty/ any other department of the hospital if the patient admitted.
iv. All MI Rooms and hospitals will maintain a MLC register and the MLC will be initiated and documented in the register. Personal particulars, identification marks, finger prints of the individual will be noted.
Particulars of the person accompanying the patient will also be noted.
Medico-legal documents should be prepared in duplicate, with utmost care giving all necessary details, preferably written with a ball-point pen and avoiding overwriting. If any overwriting or correction is made, it should be authenticated with the full signature and stamp of the MO. Abbreviations of any sort should be avoided.
v. The medical officer should not come under any pressure whatsoever and should not accede to any requests made by the patient or the persons accompanying not to register an MLC. In case of a doubt whether a particular case falls under MLC or not MLC, it is better to register it as an MLC.
⚠ Under Section 39 of Criminal Procedure Code, the attending MO is legally bound to inform the police about the arrival of an MLC. Any failure to report the occurrence of a MLC may invite prosecution under Sections 176 and / or 202 of I.P.C.
PRECAUTIONS TO BE TAKEN IN MLC:-
I. CONSENT
Consent, an important responsibility of a doctor, is defined as "Two or more persons are said to consent when they agree upon the same thing in the same sense" (Sec 13, The Indian Contract Act).
For the purpose of clinical examination, diagnosis and treatment, any person who is conscious, mentally sound and is above 18 years of age can give consent.
Consent is not legally valid when given under fear, fraud or misrepresentation of facts or is given by a person who is under 12 years.
To be valid, the consent must be competent, freely given, informed, and specific to the procedure being performed.
In medico-legal cases, an informed consent includes information that:
I. the examination to be conducted would be a medico-legal one and would culminate in the preparation of a medico-legal injury report,
II. all relevant investigations needed for the said purpose would be done,
III. the most important, the findings of the report may go against the patient if they do not tally with the history given.
IV. in all cases of sexual offences, a written consent of the victim before medical examination is mandatory even though bought by police/ investigating agency. The said examination must be done by lady MO/ preferably lady gynaecologists. Whenever examining a woman, it is preferable that a lady doctor should examine her, or, wherever this is not possible, a female attendant (nurse, etc) should be present during the examination.
Consent is not required in following condition:
A person arrested as an accused in a criminal offence may however, be medically examined without his consent on the request of a police officer or on the orders of the court, if there are sufficient grounds to believe that such examination will provide evidence of the commission of the offence.
Moreover, a reasonable amount of force may be used to medically examine the person in such cases (Sec
53 CrPC).
To invoke Sec 53 of CrPC, certain criteria need to be fulfilled, namely:
I. the person should have been arrested on charge of committing an offence punishable under law,
II. there are reasonable grounds for believing that an examination of this person will afford evidence as to the commission of the offence, and
III. the requisition for medico-legal examination is from an officer of the rank of a sub-inspector of police or above.
In the following situations, it may not be necessary to take the consent:
✦ If doctor is managing a patient in an Emergency situation;
✦ While working in situations of public interest like during floods, cyclones, earthquakes, etc;
✦ Treating patients in places like mental asylums, orphanages, and
✦ Working under Court order, e.g. in case of smuggling, operations are done for detecting narcotics or gold kept in intestine or other parts of body.
II. MEDICO-LEGAL REPORT
A Medico-legal Report (MLR) comprises of three parts, namely:
1. Pre-amble includes :-
✦ date, time and place of examination,
✦ name of the patient, his residential address, occupation;
✦ name of the person(s)/police official accompanying, Daily Docket Receipt (DDR) /FIR No.,
✦ informed consent of the person being examined, two marks of identification, etc, wherever applicable.
2. Body (Findings/Observations) includes:-
✦ a complete description of the injuries/ any other findings present;
✦ any investigations/referrals, etc, asked for.
3. Post-amble (Opinion) includes:-
✦ the nature of the injury- whether simple or grievous.
✦ weapon/force used- whether blunt or sharp or fire-arms or burns, etc.
✦ duration of the injuries- based on the characteristics of the external injuries.
✦ any other information that may prove to be helpful to the police.
✦ if for any reason, the opinion is to be kept 'pending', the same is to be documented properly in the appropriate column.
Precautions to note:-
(a) The complete available particulars of the patient should be noted down along with two identification marks. Particulars of the person accompanying the patient will also be noted down.
[In case of RTA and critically injured patients who are brought to the nearest MH/BH/GH by any civilian as Good Samaritan the details of latter is noted if they are willing to give, otherwise if they do not agree to give their details they should not be forced to furnish their details. (as per the Good Samaritan Law, Ministry of Road Transport and Highways, Govt. of India.)]
(b) One should not rely on memory while writing reports or during recording of evidence in a court of law. Complicated cases should be discussed with seniors and colleagues.
(c) The Officer/DMO/RMO, issuing the MLR register to any doctor should ensure that it is properly numbered and a certificate regarding the same (giving the number of forms contained there-in) should be given by him on the first page of the said register. All investigation forms, X-rays, Case file, etc should bear the label "MLC" on the top, so that necessary precautions can be taken by all concerned.
(d) No cause of death will be mentioned in the death certificate. The statement that "Exact cause is to be ascertained by post mortem examination" is to be endorsed.
(e) In MLCs, the body will not be handed over to the NOK / relatives. The civil police will be informed and the body handed over to them. The police will, after the medico-legal formalities, handover the body to the Next of Kin (NOK) / relatives.
(f) Death of a service person, in an accident involving a military aircraft will not be reported as a MLC to the civil police. The enquiry conducted by the competent military authorities will suffice. As per Govt of India, Ministry of Home Affairs Letter No. 8/179/71-GP A, dated 25 Nov 72, there is no need for an inquest under Section 174 or 176 of Cr PC in deaths due to an accident, in which the aircraft belongs to the Navy, Army, Air Force or Para military forces and the deceased person is an active member of any service at the time of accident. A certificate from the CO of the deceased person or a Senior Armed Forces Officer to this effect may be accepted for dispensing with the necessity of an inquest.
(g) A MLC should be reported by the first health care establishment in which the individual is received. In cases where a patient has been transferred before initiation of a report, the hospital to which he is transferred can initiate the report. It is important to ensure that the medical records are comprehensive before a patient is transferred. The fact as to whether or not medico-legal formalities have been initiated should invariably be mentioned in the transfer notes.
Confidentiality of MLRs:-
According to Hippocratic Oath and as per MCI guidelines, all doctors are required to keep secret all information regarding the patient that he comes across during the course of his treatment. Medico-legal reports are no exception and are to be treated as strictly confidential. They should not be issued directly to the patient. They have to be handed over to the police official, after getting them duly received on the carbon copy of the same. Copies of the MLR can be handed over to the patient/ his relatives, as per the prevailing rules of the hospital, and after the requisite fee has been paid by the patient.
Custody of the Records:-
The records should be kept under lock and key, in the custody of the doctor concerned or may be kept in a hospital Record Room or as per the institution's rules. Most of the hospitals have a policy of maintaining all medico-legal records for variable periods. However, as per law, there is no specified time limit after which the MLRs can be destroyed. Hence, they have to be preserved. (In view of the multitude of cases against the doctors under the Consumer Protection Act, it is advisable to preserve all the in-patient records for a period of at least 5 years and OPD records for 3 years.)
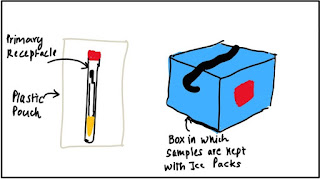
III. COLLECTION & PRESERVATION OF SAMPLES
(a) Medico-legal evidence should be preserved and subsequently sent or handed over to the investigating authorities for forensic examination and production as evidence in a court of law. All evidences will be identified, sealed and labeled properly. They will be kept in safe custody and handed over to the investigating officer of the case. A proper receipt from Police Officer should be obtained saying sample is duly sealed. Once collected, loss / destruction of evidence is a punishable offence. Failure to collect, destruction or loss of such an exhibit is punishable under Sec 201 of I.P.C.
(b) The concerned police official should also be handed over the requisition letter detailing the tests to be conducted on each samples. If in case the samples have been collected on the request of the police, the fact is to be mentioned in the report and no requisition is necessary.
(c) The evidence required to be preserved is related to the nature of a case. In injury cases, the following articles should be preserved in sealed envelopes:
✦ Clothing worn by the patient showing evidence of injury such as tears, bullet holes, cuts, blood stains etc.
✦ In case of multiple tears, cuts or holes etc., each piece of evidence will be encircled and numbered with matching description in the MLC report and case sheet.
✦ Bullets recovered from a body should be marked by etching an initial or a mark on the bottom before preservation.
✦ All evidence collected should be mentioned in medico-legal documents to establish the chain of custody in a court of law subsequently.
(d) In cases of suspected poisoning the following articles will be preserved and ensured that they are forwarded for forensic examination:
✦ Gastric lavage / gastric contents / vomitus and soiled clothing
✦ Blood, urine and any other relevant body fluid depending on the poison ingested.
(e) In cases of Burns and Carbon Monoxide poisoning the following articles should be preserved in sealed envelopes:
✦ Articles soiled with inflammable substances like burnt pieces of clothing, scalp hair etc.
✦ Blood (and not serum) for carbon-monoxide levels.
(f) In Sexual offences, the following articles should be preserved in sealed envelopes:
✦ Clothing worn by the patient and showing evidence of blood stains or seminal stains, stains of mud, tears/cuts etc.
✦ Vaginal swab preferably from posterior fornix / anal swab.
IV. DISCHARGE, REFERRAL OR DEATH IN MLC
(a) If the patient is not serious and can take care of himself, he may be discharged on his own request, after taking in writing from him that he has been explained the possible outcome of such a discharge and that he is going on his own against medical advice. Police have to be informed before the said patient leaves the hospital.
(b) While discharging or referring the patient, care should be taken to see that he receives the Discharge Card/ Referral Letter, complete with the summary of admission, the treatment given in the hospital and the instructions to the patient to be followed after discharge.
Failure to do so renders the doctor liable for "negligence" and "deficiency of service".
(c) Sometimes the patient, registered as a medico-legal case, may abscond from the hospital or not found in hospital premises. In such cases, all efforts will be first made by the hospital to locate him/her.
Information will be sent to the Civil Police and NOK regarding his/her absence from the hospital. When all efforts to locate the patient do not succeed, he/she will be discharged in absentia. After being discharged in absentia, should the patient report again to the hospital, he/ she will be re-admitted for further treatment, if required.
(d) Dying Declaration:- In cases where the patient wishes to make a dying declaration, the magistrate will be intimated. If the Magistrate is unable to come and record a statement or where the MO feels that he might not be able to reach the patient in time, the MO may record the dying declaration himself in presence of two independent witnesses whose signatures are also affixed in the document. The MO will certify the soundness of mind of the person making the dying declaration.
(e) In case of death during working hours or off-duty hours,
✦the MO in charge of the case/ DMO will have to inform immediately the Registrar/higher authorities, Next of Kin (NOK) and the civil police.
✦Civil Police is to be informed in writing with copies to all concerned.
✦Body will be handed over to civil police for further disposal.
✦Under no circumstances will the MO certify the cause of death in such cases without holding a post-mortem examination, even if there is a strong evidence the underlying cause and neither should the body be handed over to next of kin directly.
✦Alternately clearance in writing should be obtained from civil police for disposal of the body.
✦In case the body is being sent for medico-legal autopsy to civil hospital, brief summary of the case will be given to civil police. A receipt for handing over the body to police will be taken and kept along with the case documents.
(f) Instructions for preservation and safe custody of a body in mortuary until handing it over to police:-
✦The body should be properly packed at the earliest.
✦The dead body will be marked with a skin marking pencil.
✦At the time of handing over the body to the Mortuary, an identification disc will be tied to the right great toe of the deceased for easy identification, on which the name of the deceased will be written.
✦When a female dead body is transferred from the ward to the mortuary, the Medical Officer will ensure that a female attendant accompanies the body and when such transfer is done at night, a male staff is additionally detailed.
✦The mortuary staff will note down two identification marks of the deceased and confirm the particulars of the deceased as noted on the metal identification disc on the right great toe of the deceased by checking with the accompanying documents.
GUIDELINES FOR SPECIFIC MLC:-
I. MEDICO-LEGAL ASPECTS OF SEXUAL OFFENCES
(a) Victims of alleged Sexual offences like rape may be brought to the MI Room or may come on their own. In the event the victim comes directly, the civil police will be informed and necessary action will be taken to register a case. The examination may be carried out at a centre authorised for medico-legal work with forensic experts. Where the examination is carried out by a service MO, it should preferably be done by a lady MO or Gynaecologist or by MO i/c MI room in the presence of a female attendant. In cases of
sodomy, the victim may be examined by the MO i/c MI Room.
(b) Guidelines for attending alleged victim of sexual offence:-
✦ The date and time of examination will be mentioned in the case sheet. Case sheet will be initiated, noting personal particulars of the victim, along with date and the time of reporting.
✦ MLC will be initiated after filling the MLC Register available at MI Room.
✦ The alleged victim will be admitted if the medical condition is serious.
✦ The civil police will be informed telephonically followed by in writing after filling up the MLC Register. The Senior Registrar will be informed.
✦ At least two identification marks of the victim will be mentioned in the case sheet as well as in MLC register.
✦ Report to the police will be given by name of the victim or as an unknown case (If name of the victim is not known). Care must be taken to preserve the confidentiality of the victim from others not related with the case. Police will register a case under the relevant section of the IPC.
✦ The police may take the victim and the accused for medical examination at a hospital which is authorised to carry out medico-legal work.
✦ Consent of the victim must be obtained before starting the examination. The steps of examination and their purpose should be explained to the victim in a language she understands. The examination is to be carried out in the presence of a female attendant.
✦ All injuries present on the body will be recorded. Line diagrams depicting the front and back of the body may be used for a better description of location of the injuries.
✦ If the clothes are the same as those worn during the occurrence of alleged sexual offence, they should be carefully examined for the presence of blood, seminal stains, mud etc.
✦ If there are any marks of suspicious stains, the clothes should be preserved with a view to forwarding them to the Chemical Examiner of dependent Forensic Science Laboratory (FSL).
✦ If there are foreign hairs, fibers, debris under the nails etc, they must be carefully preserved and sent to experts of FSL for comparison with those found on the accused. Specimens should include vaginal swab, preferably from the posterior fornix.
✦ In case the victim reports herself directly to the hospital after the alleged crime, she should not be sent to the police station for legal formalities; instead the police will be called to the hospital for the necessary requirements.
(c) Special precautions in case of sexual offence :-
✦ The date and time of arrival of the victim must be mentioned, both in the case sheet and the MLC Register. The duplicate copy of case sheet and Medico-legal Report shall be preserved for future reference.
✦ Care must be taken to preserve various samples of medico-legal importance for their submission to respective police authority.
✦ Where the accused in a case of sexual offence in police custody is brought for medical examination, consent is not required. Samples may be collected and handed over to the police for forensic examination.
✦ All injuries shall be recorded in cases of alleged victims of sodomy.
✦ Care must be taken to preserve the vaginal / anal swab for forensic examination.
✦ Neither the victim nor accused in cases of sexual offences should be permitted to wash or take a bath till the medical examination is completed.
II. MEDICO-LEGAL ASPECTS OF POISONING
(a) Poison may be defined as any substance which when absorbed into the body or by local action on the tissues injures health or destroys life.
(b) Medico-legal aspects of Poisons. Sections 284, 299, 300, 304A, 324, 326 and 328 of IPC deal with offences relating to handling and administration of Poisonous substances. As per Indian law, administration of any substance with the intention of causing hurt or death is punishable.
(c) Guidelines in case of Poisoning:-
✦ When poisoning is suspected, every attempt must be made to save the patient's life. The patient shall be shifted immediately to the hospital / MI room nearby.
✦ Case sheet shall be initiated, noting personal particulars of the victim, along with date and time of reporting. The particulars of the person accompanying the patient will also be noted.
✦ The victim will be protected from further exposure of poisoning but no clothing shall be thrown away, as they might be useful for chemical analysis.
✦ MLC will be initiated after filling the MLC Register available at MI Room. Registrar of the hospital and Civil police must be informed.
✦ The patient will be admitted if the medical condition is serious.
✦ The treating doctor / authorised nursing staff will only be permitted to administer food and medicines to the patient.
✦ A careful history is to be elicited including relationship of food or medicine taken and the toxic manifestations. All signs and symptoms are to be noted carefully.
✦ The vomitus, urine, faeces, stomach wash, sample of food or medicine taken should be preserved in a sterile bottle. Any suspicious bottle or utensil seen near the victim, the clothes and bed clothes used last by the victim are all to be preserved for chemical analysis. Suitable preservatives may be used for these purposes depending upon the nature of the sample. The name and concentration of preservative used should invariably be mentioned in the label and / or accompanying documents.
✦ It is advisable to take the second opinion and advice of a senior professional colleague in all matters regarding diagnosis and treatment. Use of Poison information services may also be made.
✦ If there is any indication of danger to the general public, for example, food poisoning from a hotel, the public health authorities must be notified at once so that suitable remedial measures are taken.
✦ Where required, a magistrate should be called to take down the dying declaration.
(d) Precautions to be taken in cases of poisoning:-
✦ Emergency medical treatment will be administered. Senior colleagues will be consulted and Poison Information Services will be made use of wherever available.
✦ Medical certification and cause of death will be issued with mention that 'Cause of death to be ascertained after chemical analysis'.
✦ Various samples of medico-legal importance will be preserved and handed over to the police for forensic examination.
✦ A receipt shall be obtained from the police for all samples that are handed over for forensic examination.
III. GUIDELINES IN CASE OF MEDICAL MISHAP
(a) The patients and their relatives expect a kind and compassionate attitude from a doctor. A scientifically sound approach, good behaviour and care of a reasonable standard usually protect a Medical Officer from professional complaints.
(b) There are occasions when something untoward happens following a diagnostic or therapeutic procedure. In such a situation, the physician must take the following steps: -
✦ Complete the patient's record and recheck the written notes.
✦ Be honest and inform about the mishap. Show genuine concern about the unfortunate incident. Answer all the queries of patient / relatives. Doctors, who are open-minded and communicative, are much less likely to face complaints.
✦ The doctor may contact other doctors, Forensic Medicine experts and professional protection bodies to seek advice.
IV. MEDICAL NEGLIGENCE (MALPRACTICE)
(a) Medical negligence or malpractice is defined as "lack of reasonable care and skill or wilful negligence on the part of a doctor in the treatment of a patient whereby the health or life of a patient is endangered". The term "damage" means mental or functional injury to the patient, while "damages" are assessed in terms of money by the court on the basis of loss of concurrent and future earnings, treatment costs and reduction in qualities of life.
(b) In order to establish charges for negligence, the following points are required to be established to the satisfaction of the court, by the consumer, that:
✦ The doctor (defendant) owed him a Duty to conform to a particular standard of professional conduct.
✦ The doctor breached that duty. (Dereliction)
✦ The doctor's conduct was the Direct Cause of the damage.
✦ The patient suffered actual Damages.
(c) The burden of establishing all above elements is upon the patient / consumer. Failure to provide substantial evidence on any one element may result in "No compensation".
(d) In an emergency situation the medical officer has to attend the patient at the place where the patient is, if the medical condition so warrants. Inability to do so without a valid reason will constitute medical negligence.
(e) Criminal Negligence:- Here the negligence is so great as to go beyond a matter of mere compensation; not only the doctor has made the wrong diagnosis and treatment, but he has shown gross ignorance, gross carelessness or gross neglect for life and safety of the patient. For this, the doctor may be prosecuted in a criminal court for having caused injury or death of the patient by a rash and negligent act amounting to culpable homicide under Sec 304-A of Cr. P.C., under following conditions:
✦ Injecting anaesthetic in fatal dosage or in wrong tissues
✦ Amputation of wrong finger, operation on wrong limb, removal of wrong organ etc.
✦ Operation on wrong patient
✦ Leaving instruments or sponges inside the part of body operated
✦ Leaving tourniquet too long resulting in gangrene
✦ Transfusing wrong blood
✦ Applying too tight plaster or splints, which may cause gangrene or paralysis
✦ Performing a criminal abortion.
V. GENERAL GUIDELINES FOR SUDDEN DEATH/FOUND
DEAD CASES
(a) Deaths, which require medico-legal investigation, may be divided into three main groups: -
✦ Deaths either known or suspected to have been caused by unnatural causes.
✦ Sudden death cause unknown.
✦ Found dead – Unattended death.
(b) As per ICD 10, "sudden death cause unknown" could be as follows:-
• R96.0 - Instantaneous death
• R96.1 - Death occurring less than 24 hours from onset of symptoms, not otherwise explained
• R98 - Death in circumstances where the body of the deceased was found and no cause could be
discovered. Found dead.
• R99 – Death NOS (Not Otherwise Specified). Unknown cause of mortality.
(c) Deaths due to natural causes fall within the medico-legal domain when they occur in custody, clashes, accidents and sometimes even during violent arguments. Therefore a Medical Officer should not certify the cause of death in such cases without holding a post mortem examination, even if there is strong evidence of the underlying cause.
(d) The deceased will be examined in detail by attending MO and resuscitation will be attempted, failing which death will be confirmed. Two identification marks will be noted.
(e) Circumstances leading to death will be ascertained from person bringing and identifying the body.
(f) All particulars and address of the person(s) bringing the deceased will be noted in the case sheet and history given by them will be endorsed in the case sheet as alleged history.
(g) MO i/c MI Room / DMO will immediately inform higher authorities and NOK and civil police. Civil Police is to be informed in writing with copies to all concerned.
(h) Body will be handed over to civil police for further disposal. Under no circumstances will the body be handed over to next of kin directly. Alternately clearance in writing should be obtained from civil police for disposal of the body.
(i) In case the body is being sent for medico-legal autopsy to civil hospital, brief summary of the case will be given to civil police. A receipt for handing over the body to police will be taken and kept along with the case documents.
CONCLUSION:-
Proper documentation, timely information, a methodological and thorough examination including all relevant investigations and referrals, etc. pertaining to medico-legal cases must be handled tactfully by the MOs following the institution's prevailing guidelines. The administrative authorities must also help in maintaining goodwill and avoiding legal complications. It is hoped that this collation of directives on handling of medico-legal issues will act as a safeguard against procedural lapses.
CREDITS:-
2. Dr. Omna Shaki, Dr. SK Rai in International Journal of Scientific Research, Vol. 6, Issue 9 on An approach to Medico-legal cases in Indian Government hospital "Do's and Don'ts", September 2017.
Written by our guest author Pranav Survase
#Ae(ONE)INTERN