- Spontaneous onset - At term
- Vertex presentation
- Without undue prolongation
- Natural termination with minimal aids
- Without any complications
ADMISSION:
1. Admit in waiting ward if in early labor OR admit in Labor Ward if cervix > 4 cm dilated, uterine activity is optimum, show, and/or spontaneous rupture of membranes present. Delay transfer to the labor ward until in active labor (i.e., equal to or greater than 4 cm dilatation practically) is established
2. Confirm reports of Hemoglobin, blood group, VDRL, plasma sugar (fasting and postprandial or random), HIV, HBsAg, urinalysis, TSH, and obstetric ultrasonography are ready and normal. If not, get them done without compromising care
3. Check if she has received tetanus immunization. If the patient is not immunized and directly presents during labor, give tetanus immunization to her immediately and the child after delivery is given tetanus immunoglobulin
4. Send blood for cross matching only if there is an indication for the same
FIRST STAGE:
From true labor pains to full cervical dilatation. (≈10 cm)
Foetal heart rate (FHR) is monitored every 30 mins in first stage, 15 mins in second stage.
In high risk pregnancies, FHR is monitored every 15 mins in first stage, 5 mins in second stage.
Orders
● Shave/ clip hair and prepare private parts
● Simple enema stat
● Left lateral position
● Liquids/ soft diet orally
● MATERNAL VITAL SIGNS: Temperature, pulse and blood pressure are evaluated at least every 1/2 hourly
● SUBSEQUENT CERVICAL EXAMINATIONS: Cervical dilatation and presenting part evaluated by PV every 4 hours
● ORAL INTAKE: Food should be withheld during labor and delivery as gastric emptying is remarkably prolonged once labor is established/ analgesia is given
-Sips of clear fluids (or fruit juices) are permitted to prevent dehydration
-Allow a gravida at low risk of requiring general anesthesia to eat low residue food or drink as desired or tolerated
-Usually a pint of Ringer Lactate also given to the patient
● URINARY BLADDER FUNCTION: Mother should void the bladder if possible, else catheterize and drain the urine using a simple red rubber catheter. (Distension of bladder is to be avoided as it can interfere with the fetal presenting part and lead to subsequent bladder hypotonia and infection)
Consider amniotomy in active phase of labor (done by senior residents, not expected from interns).
If the membranes are ruptured, IV antibiotic is started.
SECOND STAGE:
With full cervical dilatation and engaged presenting part, encourage the patient to bear down when the female feels the urge to push (with each uterine contraction).
Permit delay in pushing when the presenting part is above station +2, occiput is not in anterior position, as long as the fetus is well.
The woman should be allowed to push with open or closed glottis (Valsalva manoeuvre) according to her preference.
Continue intrapartum monitoring.
PREVENTION OF PERINEAL TEARS:
● Application of warm perineal compresses: relaxes the muscles
● Perineal massage
● Provide perineal support when head is coming out
● Avoid routine episiotomy (Although this is routinely done in most of the government hospitals)
● Avoid fundal pressure
EPISIOTOMY: Done under pudendal nerve block using lignocaine during crowning when the head descends down (baby is being pushed). Cut at the time of contraction only. Mediolateral episiotomy at 60 degree on a stretched perineum is given using episiotomy scissors.
Delivering the Baby: Ask a person to provide urethral support (put index and middle finger in the vagina against the anterior vaginal wall) while you provide perineal support (put index fingers of both your hands inside the vagina and stretch it downwards and laterally).
Do modified RITGEN manoeuvre (Perineal support plus hand on occiput to cause controlled extension of head means the head is delivered in extension and trunk by lateral flexion).
Immediately ask the sister to give oxytocin 10 IU given i.m
If i.v. line already in-situ, 10 IU of oxytocin is injected into the RL pouch
Delay umbilical cord clamping for 1 minute or till cord pulsations stop if the newborn does not require neonatal resuscitation or is not a case of Rh isoimmunization.
● During this time, encourage maternal-neonatal skin to skin contact provided there are no maternal or neonatal complications while drying the neonate. Place the naked term infant on the mother's bare abdomen and cover them with a clean warm sheet.
● Touch the cord to check if the pulsation stops. After this, three Kocher's clamps are applied on the cord (2 towards the baby and 1 towards the placenta) and the cord is cut in between ( Provides extra 80 ml of blood to fetus).
● After this the baby is handed over to the neonatologist. In case of foetal distress, early cord clamping is done and then the neonatologist takes the charge
THIRD STAGE :
Hand placed over the fundus and look for signs of placental separation:
1) Increase in fundal height
2) Gush of blood
3) Permanent elongation of umbilical cord
4) Suprapubic bulging (most important)
The uterus may be massaged
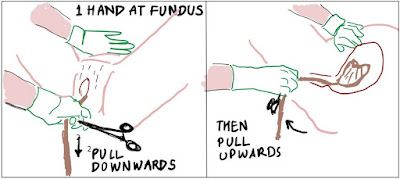
• Placental expulsion is done by Brandt Andrews Method (Controlled cord traction) after signs of placental separation
(a) Apply traction on the part of the cord outside the vulva, first downwards with one hand supporting the fundus of the uterus (to prevent uterine inversion), and then guiding it upwards and out of the birth canal once separation has occurred.
(b) Wrap the excess length of the cord coming out around the clamp.
(c) Repeat (a).
• Once the placenta appears at the vulva, both hands are used to hold and twist it gently to ensure that all the membranes are delivered intact
• Inspect placenta to ensure no part is retained inside
• Check the tone of the uterus: Contracted uterus should feel rock solid
• If the uterus is not contracting, then ask the sister to give Oxytocin. If this fails, 800-1000 µg of Misoprostol is given per-rectally. If this fails, Carboprost 125 µg is given i.m. Do keep in mind the contra-indications of the latter two. Even after all this if the uterus does not contract, call a senior immediately
Following this, the vulva and vagina are carefully inspected and repaired if necessary.
Episiotomy is sutured in 3 layers using Chromic catgut (0) preferably or else Rapid Vicryl:
1. Continuous interlocking suture is taken beginning from 1cm above the apex of vaginal mucosa till the muco-cutaneous junction
2. Simple interrupted suture for the muscle
3. Vertical mattress suture or subcuticular for the skin
Sterile pad is applied.
FOURTH STAGE:
• The patient is shifted to the side room. She is allowed to take everything (solids/liquids) by mouth just like a normal patient
• Record the following after 1 hour: Pulse, temperature, blood pressure, tone of the uterus to be monitored. Check episiotomy scar for vulval hematoma
• Look for abnormal vaginal discharge and excess bleeding
• She is instructed not to sit cross-legged but with the extended legs for the risk of wound gaping
• The patient is asked to go to the washroom and empty her bladder. This is to ensure that there is no urinary retention, after which she is shifted to the ward
Episiotomy wound care: metronidazole+ povidone ointment iodine / povidone iodine ointment is applied 4 times/day. For excess pain, lignocaine gel is given and the patient is advised sitz bath
She is prescribed the following antibiotics generally:
a) Amoxicillin-Clavulinic acid 625 mg TDS
b) Metronidazole 400 mg TDS
c) PPI (Pantoprazole40 mg) OD
Usually the patient is discharged on the 3rd day
Written by our guest authors Konal Ahire, Mithil Rathod and Ayushi Gupta Illustrations by Anveshi Nayan
#Ae(ONE)INTERN